Introduction
Sickle cell trait (SCT) is a genetic condition that affects millions of people globally, particularly those of African and Mediterranean descent. Various mechanisms have been suggested to contribute to cardiovascular pathology in SCT patients, including chronic anemia, arteriopathy, and cardiac remodeling. However, whether SCT carriers, particularly African Americans (AA), are at an increased risk for cardiovascular disease remains controversial. This study aimed to investigate potential differences in cardiovascular outcomes between AA and non-AA SCT carriers.
Methods
We screened the National Inpatient Sample (NIS) database 2016-2018 for cardiovascular outcomes during hospital admission in African American SCT carriers and compared them to SCT carriers of other races. The primary outcomes were major adverse cardiovascular events, including acute myocardial infarction, cardiac arrest, stroke, acute heart failure, and in-hospital mortality. Secondary outcomes included World Health Organization (WHO) group 5 pulmonary hypertension, acute pulmonary edema, valvular disease, pericarditis, tachyarrhythmia, conduction disorders, acute deep venous thrombosis and/or pulmonary embolism, avascular necrosis, and rhabdomyolysis. Univariate analysis was conducted, with a P value <0.05 considered statistically significant.
Results
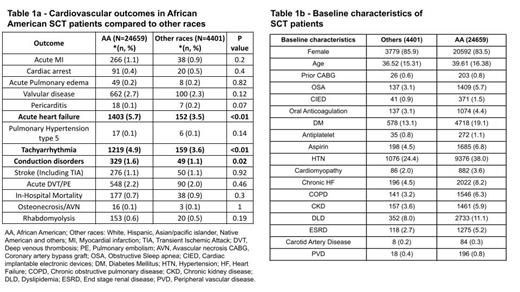
A total of 29,060 SCT admissions were analyzed, with 24,659 attributed to African Americans and the remaining to other races. The study found that majority of the patients admitted were female (86% of African American patients and 84% of patients from other races). The average age of patients was 37 years for African Americans and 40 years for other races. African American patients had higher rates of comorbidities such as hypertension, diabetes, chronic kidney disease, and oral anticoagulant use compared to patients of other races.
The study also found that African American SCT patients had a significantly higher risk of acute heart failure (5.7% vs. 3.5%, p<0.01), tachyarrhythmia (4.9% vs. 3.6%, p<0.01), and conduction disorders (1.6% vs. 1.1%, p=0.02) compared to patients of other races. Acute myocardial infarction (1.1% vs. 0.9%), valvular disease (2.7% vs. 2.3%), acute deep vein thrombosis/pulmonary embolism (2.2% vs. 2.0%), and rhabdomyolysis (0.6% vs. 0.5%) occurred at a higher rate in African American patients but did not reach statistical significance. Similarly, in-hospital mortality (0.7% vs 0.9%), cardiac arrest (0.4% vs 0.5%), and pericarditis (0.1% vs 0.2%), although occurring at lower rates in the AA population, did not reach statistical significance. Acute pulmonary edema (0.2% vs 0.2%), pulmonary hypertension (group 5) (0.1% vs 0.1%), stroke (1.1% vs 1.1%) and avascular necrosis (0.1% vs 0.1%) had similar rates in both AA and other races but did not reach statistical significance.
Conclusion/Discussion
African American patients with sickle cell trait compared to other races had higher rates of acute heart failure, tachyarrhythmias, and other conduction disorders. Aggressive screening for cardiac conditions and management of risk factors including smoking, obesity, high blood pressure, hyperlipidemia, etc., are warranted in this population to improve cardiovascular outcomes. Although the NIS database provides this study with large patient data, this study may be limited by difference in the number of patients in AA and other race cohorts at baseline, coding error, underreporting, misclassification, retrospective nature, and lack of matching. Further studies analyzing the cardiovascular morbidity and mortality in sickle cell trait carriers, including benefit of use of medications for primary/secondary prevention of cardiovascular conditions are warranted.
Disclosures
Ogu:Vertex Pharmaceuticals: Consultancy; Bluebird Bio: Consultancy; Emmaus: Speakers Bureau; Global Blood Therapeutics/Pfizer: Speakers Bureau.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal